COVID-19 cases are falling, but hospitals still feel the crunch
COVID-19 infections in Los Angeles are plummeting, California’s mask mandate is coming off and kids under 5 could soon be eligible for vaccination.
But inside some of the region’s hospitals, an atmosphere of crisis prevails, as medical staff contend with depleted ranks and a heavy caseload.
COVID-19 hospitalizations in Los Angeles County hit a winter peak of 4,814 patients on Jan. 20. Although they have been on the decline ever since, the situation remains serious: As of Feb. 1, 20% of all COVID-positive hospitalized patients were in the intensive care unit. According to the Los Angeles County Department of Public Health, 14% required ventilation.
COVID-19 hospitalizations in Los Angeles County
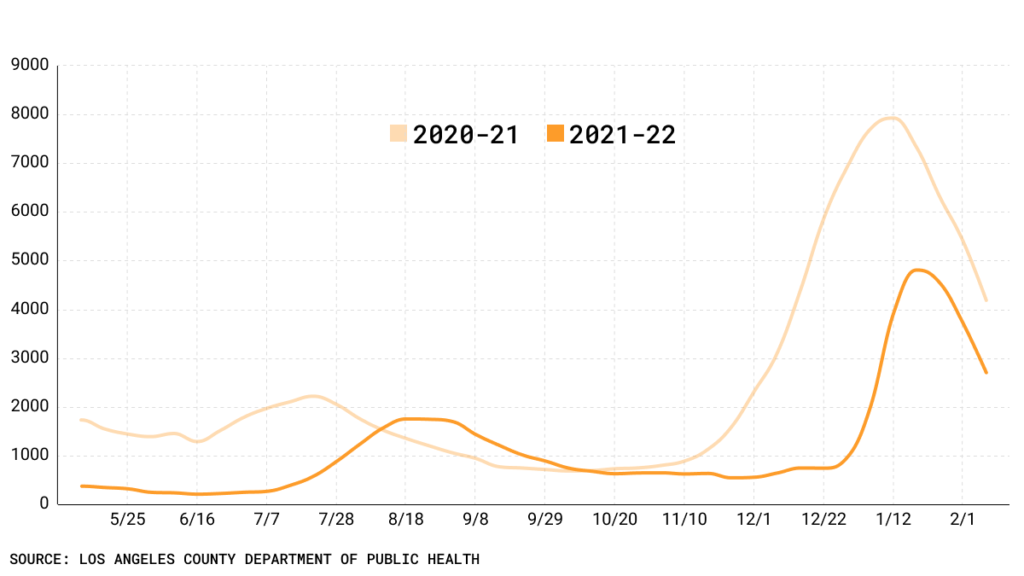
On Thursday, there were 2,464 COVID-19 patients in area hospitals.
The strain extends to the four public hospitals under the auspices of the Los Angeles County Department of Health Services. As of Feb. 5, the facilities reported 282 patients who had tested positive (regardless of why they were admitted). Fifty-five ICU beds were occupied by COVID-positive patients.
Working in overcrowded and understaffed hospitals has driven some healthcare workers to the brink of exhaustion. That includes Dr. Nancy Blake, chief nursing officer at Los Angeles County + USC Medical Center in Lincoln Heights.
“It has been tough to watch the destruction this disease has inflicted on our entire community, including our patients and their families, as well as our staff and their families,” Blake said.
Labor shortage
LAC + USC Medical Center is one of the many facilities facing an extreme shortage of staff due to an increase in COVID-19 cases among healthcare workers. Although numerous doctors, nurses and support personnel are returning to work, some patients in need of medical attention have suffered.
“Over the holidays, there were days when there were 177 in-patient beds open but unstaffed due to nursing shortages,” said Dr. Emily Rose, a pediatric emergency medicine specialist at LAC + USC Medical Center. “Patients were waiting for 20-plus hours in our waiting room to be seen. That was horrific.”
Adding to the problem is that many hospitals are struggling to recruit staff, given the long hours and high risk of virus exposure. On Tuesday, the California Medical Association asked Congress to provide more support to physicians and their staff, and wrote, “The second year of the pandemic truly tested physician stamina.”
Dr. David Belson, an expert in hospital efficiency and a professor at the University of Southern California Keck School of Medicine, echoed the concern.
“People find the work really difficult and burdensome and stressful,” said Belson. “So it’s hard to get people and there are less people available.”
[Get COVID-19, crime and other stats about where you live with the Crosstown Neighborhood Newsletter]
Out sick
The Omicron spike presented challenges for people across the United States and around the world. Although many of those infected endured milder symptoms than patients did in earlier waves of the pandemic, the high transmissibility meant that a large number of healthcare workers who contracted COVID-19 had to quarantine.
More than 3,200 county medical staff tested positive for COVID-19 during the Omicron surge, and during the course of the pandemic, at least 55,675 healthcare and frontline workers have contracted the disease, according to the County Department of Public Health.
In the effort to reduce cases among hospital staff, all booster-eligible healthcare workers in the county were required to get their third dose by Feb. 1. The mandate came in the wake of evidence of the booster’s effectiveness in reducing infection rates, hospitalizations and deaths.
How we did it: We examined coronavirus data provided by the Los Angeles County Department of Public Health, as well as hospital data from the Los Angeles County Department of Health Services.
Interested in our data? Check out the Crosstown coronavirus interactive map or email askus@xtown.la.